One man turned nursing home design on its head when he created this stunning facility
"What if we design an environment that looks like outside?" he said. "What if I can have a sunrise and sunset inside the building?

92-year-old Norma had a strange and heartbreaking routine.
Every night around 5:30 p.m., she stood up and told the staff at her Ohio nursing home that she needed to leave. When they asked why, she said she needed to go home to take care of her mother. Her mom, of course, had long since passed away.
Behavior like Norma's is quite common for older folks suffering from Alzheimer's or other forms of dementia. Walter, another man in the same assisted living facility, demanded breakfast from the staff every night around 7:30.
Jean Makesh, CEO of Lantern assisted living facilities, says he meets folks with stories like these every day. It's their stories that inspired him to make some changes at Lantern.
"I thought I knew a lot about elderly care. The more and more time I was spending with my clients, that's when I realized, 'Oh my god, I have no clue.'"
Confusion is common in Alzheimer's patients, but Makesh knew there had to be some way to minimize these conflicts.
A big believer in the idea that our environment has an enormous effect on us, he started thinking big — and way outside the box.
"What if we design an environment that looks like outside?" he said. "What if I can have a sunrise and sunset inside the building? What if I'm able to have the moon and stars come out? What if I build a unit that takes residents back to the '30s and '40s?"
And that was just the beginning. He also researched sound therapy. And aromatherapy. And carpet that looked like grass. No idea was off-limits.
What he came up with was a truly unique memory-care facility. And after testing the concept in Lantern's Madison, Ohio, facility, Makesh is opening two new locations this year.
Instead of rooms or units, each resident gets a "home" on a quiet little indoor street reminiscent of the neighborhoods many of them grew up in.

All photos courtesy of Lantern
Instead of a boring panel ceiling, residents look up and see a digital sky, which grows dimmer late in the day to help keep their biological clocks in tune.

Throughout the day, nature sounds and fresh aromas like peppermint or citrus are piped in.
Some studies have shown that this kind of aromatherapy may indeed have some merits for improving cognitive functioning in Alzheimer's patients.

There's even a little "main street" where residents can gather.
For Makesh, this isn't just about making patients comfortable, though. He wants to change how we think about the endgame of severe dementia.

The insides of the rooms aren't too shabby, either.
Makesh said one of the frustrating shortcomings of most nursing facilities is that they create conflicts with unnatural environments and schedules, and they try to solve them by throwing antipsychotic and anti-anxiety medications at patients. In other words, when someone has severe dementia, we often give up on them. From there, they stop getting the engagement their brain needs to thrive.
Of course, we're a long way from a cure for Alzheimer's.
But Makesh's project shows that when we think strategically about altering the environment and focus on helping people relearn essential self-care and hygiene skills, the near-impossible becomes possible.
"In five years, we're going to [be able to] rehabilitate our clients where they can live independently in our environment," he said. "In 10 years, we're going to be able to send them back home."
He knows it's a lofty goal. And whether he'll meet it remains to be seen. But in the meantime, he's proud to own one of the few places that offers something pretty rare in cases of severe dementia: hope.
This article originally appeared on 09.08.16




 Baby boomer grandparents.via
Baby boomer grandparents.via  A stressed mom with her head in her hands.via
A stressed mom with her head in her hands.via  A stressed mom doing laundry.via
A stressed mom doing laundry.via  A father does his daughter's hair
A father does his daughter's hair A father plays chess with his daughter
A father plays chess with his daughter A dad hula hoops with his daughterAll illustrations are provided by Soosh and used with permission.
A dad hula hoops with his daughterAll illustrations are provided by Soosh and used with permission. A dad talks to his daughter while working at his deskAll illustrations are provided by Soosh and used with permission.
A dad talks to his daughter while working at his deskAll illustrations are provided by Soosh and used with permission. A dad performs a puppet show for his daughterAll illustrations are provided by Soosh and used with permission.
A dad performs a puppet show for his daughterAll illustrations are provided by Soosh and used with permission. A dad walks with his daughter on his backAll illustrations are provided by Soosh and used with permission.
A dad walks with his daughter on his backAll illustrations are provided by Soosh and used with permission. a dad carries a suitcase that his daughter holds onto
a dad carries a suitcase that his daughter holds onto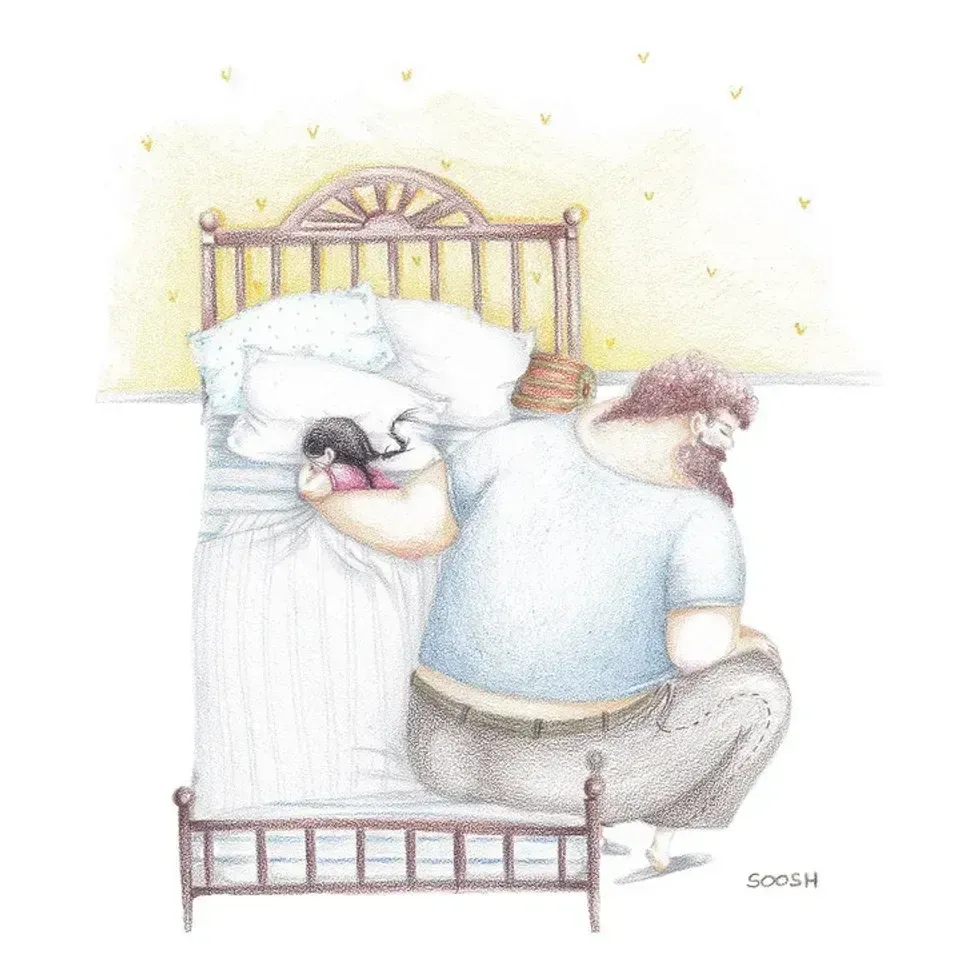 A dad holds his sleeping daughterAll illustrations are provided by Soosh and used with permission.
A dad holds his sleeping daughterAll illustrations are provided by Soosh and used with permission. A superhero dad looks over his daughterAll illustrations are provided by Soosh and used with permission.
A superhero dad looks over his daughterAll illustrations are provided by Soosh and used with permission. A dad takes the small corner of the bed with his dauthterAll illustrations are provided by Soosh and used with permission.
A dad takes the small corner of the bed with his dauthterAll illustrations are provided by Soosh and used with permission. TikTok · Kyle | Website Landlord
TikTok · Kyle | Website Landlord